Total Contact Cast Helps With Foot Ulcers

Foot ulcers can be a debilitating condition, common among individuals with diabetes. An effective treatment option in managing foot ulcers is a total contact cast. A podiatrist can apply this device and it consists of a custom-made cast that snugly conforms to the shape of your foot and ankle. The cast ensures pressure redistribution across the ulcer, reducing the risk of further tissue damage and accelerating the healing process. It also immobilizes the foot, preventing excessive movement that can worsen ulcers and hinder recovery. Further, a total contact cast acts as a protective shield, safeguarding your foot from external factors and reducing the risk of infection or other complications. Studies show that this type of cast can speed up ulcer healing compared with more conventional dressings and offloading techniques. This is due to a customized fit that maximizes both comfort and effectiveness. To determine whether a total contact cast is suitable for your condition, it is suggested that you make an appointment with a podiatrist, who is specifically trained to manage diabetic foot ulcers.
Diabetic foot care is important in preventing foot ailments such as ulcers. If you are suffering from diabetes or have any other concerns about your feet, contact Pasquale Cancelliere, DPM from Candria Foot and Ankle Specialists. Our doctor can provide the care you need to keep you pain-free and on your feet.
Diabetic Foot Care
Diabetes affects millions of people every year. The condition can damage blood vessels in many parts of the body, especially the feet. Because of this, taking care of your feet is essential if you have diabetes, and having a podiatrist help monitor your foot health is highly recommended.
The Importance of Caring for Your Feet
- Routinely inspect your feet for bruises or sores.
- Wear socks that fit your feet comfortably.
- Wear comfortable shoes that provide adequate support.
Patients with diabetes should have their doctor monitor their blood levels, as blood sugar levels play such a huge role in diabetic care. Monitoring these levels on a regular basis is highly advised.
It is always best to inform your healthcare professional of any concerns you may have regarding your feet, especially for diabetic patients. Early treatment and routine foot examinations are keys to maintaining proper health, especially because severe complications can arise if proper treatment is not applied.
If you have any questions please feel free to contact our offices located in Londonderry, NH and Salem, NH . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Exploring the Bones and Joints of the Foot

The structure of the foot comprises a fascinating network of bones and joints that enable us to walk, run, and stand. The foot has three major sections: the forefoot, midfoot, and hindfoot. The forefoot contains metatarsal bones forming the ball of the foot, while the midfoot houses various tarsal bones. The tarsal bones are responsible for maintaining arches and facilitating flexibility. The hindfoot houses the heel bone, or calcaneus, and is crucial for absorbing shock during movement. Other joints in the foot, like the ankle joint and the subtalar joint, allow for complex motions that include dorsiflexion and plantarflexion. Understanding this skeletal framework is essential for appreciating the importance of proper foot care and maintaining overall mobility and comfort. If you would like more information about the biomechanics of the feet, it is suggested that you consult with a podiatrist who can provide you with the knowledge you are seeking.
If you have any concerns about your feet, contact Pasquale Cancelliere, DPM from Candria Foot and Ankle Specialists. Our doctor can provide the care you need to keep you pain-free and on your feet.
Biomechanics in Podiatry
Podiatric biomechanics is a particular sector of specialty podiatry with licensed practitioners who are trained to diagnose and treat conditions affecting the foot, ankle and lower leg. Biomechanics deals with the forces that act against the body, causing an interference with the biological structures. It focuses on the movement of the ankle, the foot and the forces that interact with them.
A History of Biomechanics
- Biomechanics dates back to the BC era in Egypt where evidence of professional foot care has been recorded.
- In 1974, biomechanics gained a higher profile from the studies of Merton Root, who claimed that by changing or controlling the forces between the ankle and the foot, corrections or conditions could be implemented to gain strength and coordination in the area.
Modern technological improvements are based on past theories and therapeutic processes that provide a better understanding of podiatric concepts for biomechanics. Computers can provide accurate information about the forces and patterns of the feet and lower legs.
Understanding biomechanics of the feet can help improve and eliminate pain, stopping further stress to the foot.
If you have any questions please feel free to contact our offices located in Londonderry, NH and Salem, NH . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
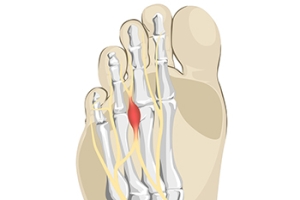
What Causes Morton’s Neuroma?
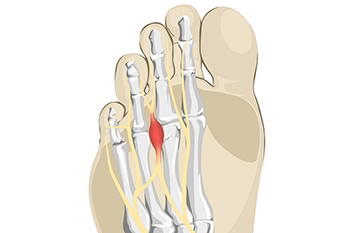
The foot condition that is known as Morton’s neuroma is painful. It is caused by wearing shoes that do not have enough room in the toe area and it affects the nerve between the third and fourth toes. High heels can fall into this category, and women can develop this condition if high heels are worn often and for long periods of time. Patients may feel this affected nerve can be malignant, however, it is considered to be a benign growth. The pain is often felt in the ball of the foot, and it may be difficult to walk. Temporary relief may be found when wider shoes with lower heels are worn. There may be swelling that accompanies this ailment, and it can be helpful to elevate the feet. In severe cases, some patients may choose surgery that can remove the nerve, and normal activities may be resumed. If you have foot pain from for Morton’s neuroma, it is strongly suggested that you contact a podiatrist who can effectively diagnose and offer the correct treatment methods.
Morton’s neuroma is a very uncomfortable condition to live with. If you think you have Morton’s neuroma, contact Pasquale Cancelliere, DPM of Candria Foot and Ankle Specialists. Our doctor will attend to all of your foot care needs and answer any of your related questions.
Morton’s Neuroma
Morton's neuroma is a painful foot condition that commonly affects the areas between the second and third or third and fourth toe, although other areas of the foot are also susceptible. Morton’s neuroma is caused by an inflamed nerve in the foot that is being squeezed and aggravated by surrounding bones.
What Increases the Chances of Having Morton’s Neuroma?
- Ill-fitting high heels or shoes that add pressure to the toe or foot
- Jogging, running or any sport that involves constant impact to the foot
- Flat feet, bunions, and any other foot deformities
Morton’s neuroma is a very treatable condition. Orthotics and shoe inserts can often be used to alleviate the pain on the forefront of the feet. In more severe cases, corticosteroids can also be prescribed. In order to figure out the best treatment for your neuroma, it’s recommended to seek the care of a podiatrist who can diagnose your condition and provide different treatment options.
If you have any questions, please feel free to contact our offices located in Londonderry, NH and Salem, NH . We offer the newest diagnostic and treatment technologies for all your foot care needs.
How MLS Laser Therapy Sheds Light on Pain and Inflammation
MLS (Multiwave Locked System) Laser Therapy is a non-invasive method of treatment that uses two continuous therapeutic wavelengths of light that penetrate deep into the tissue to stimulate the regeneration of cells, decrease pain and inflammation, and improve circulation to the injured area. While there may be a slight warming sensation at the site of treatment, the combination of these two synchronized wavelengths minimizes the risk of thermal damage. Treatments generally take 10-15 minutes, and the typical course of treatment entails roughly 6 to 12 treatments. Many patients experience long-term positive results from MLS Therapy, as it addresses the cause of pain rather than simply masking symptoms. Podiatrists may use MLS therapy to treat plantar fasciitis, Achilles tendon issues, bursitis, neuromas, arthritis, fractures, injuries, and more. If you have any of these conditions, talk to your podiatrist to see if you are a good candidate for MLS Laser Therapy.
MLS Laser Therapy is a successful alternative for treating any pain you may be experiencing related to certain podiatric conditions. If you are interested in MLS Laser Therapy, consult with Pasquale Cancelliere, DPM from Candria Foot and Ankle Specialists. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
MLS Laser Therapy
Multiwave Locked System (MLS) Laser Therapy is a patented, FDA-cleared technology that helps relieve pain and inflammation from a number of podiatric conditions, including:
- Heel Pain
- Plantar Fasciitis
- Sports Injuries
- Wounds
- Achilles Tendonitis
- Arthritis
- Neuropathy
- Neuromas
MLS Laser Therapy is an ideal alternative to surgery and prescription medication, as it has no negative side effects and encourages accelerated healing. Among its many clinical benefits, MLS Laser Therapy also:
- Reduces swelling due to bruising or inflammation
- Blocks pain
- Reduces formation of scar tissue
- Improves nerve function
If you have any questions, please feel free to contact our offices located in Londonderry, NH and Salem, NH . We offer the newest diagnostic and treatment technologies for all your foot care needs.
MLS Laser Therapy
MLS Laser Therapy is an FDA-approved technology designed to treat various painful conditions. It is often sought out as a successful alternative to surgical treatment and prescription medication that may otherwise bring about negative side effects. During MLS Laser Therapy, light energy enters the damaged cells to stimulate intercellular activity, reducing pain in the affected area and accelerating the recovery process.
MLS Laser Therapy is used in podiatry to treat various conditions. These include heel pain, plantar fasciitis, sports injuries, wounds, Achilles tendonitis, arthritis, neuromas, neurological pain, musculoskeletal disorders, and sore muscles. Aside from the specific conditions MLS Laser Therapy treats, patients can also gain from the treatment’s general benefits. These benefits include a rapid relief of pain, the reduction of swelling caused by inflammation or bruising, faster healing, improved blood circulation, the reduction of scar tissue, and improved nerve function.
MLS Laser Therapy is a non-surgical treatment with no side effects. The treatment process is painless and typically takes a short amount of time to complete. Several treatments may be required depending on the specific condition.
Requirements to Become a Podiatrist

Becoming a podiatrist, who is a specialized medical professional focusing on foot and ankle health, involves a well-defined educational journey. An interested student will typically need to complete a bachelor's degree in a related field, such as biology or premed. After this foundation, a Doctor of Podiatric Medicine, or DPM, degree is obtained, which is a comprehensive four-year program. During the DPM program, the subjects studied can include anatomy, physiology, and podiatric medicine, accompanied by clinical training. This phase will provide hands-on experience and exposure to various foot and ankle conditions. Following graduation, the competent student will likely complete a residency program, which can last from two to four years, focusing on specialized areas, such as surgery or sports medicine. The final step is to obtain licensure by passing state-specific exams. Becoming a podiatrist requires dedication, a strong educational foundation, and a commitment to promoting foot health. If you have questions about the field of podiatry, it is suggested that you confer with a podiatrist who can provide you with pertinent information.
If you are experiencing pain in the feet or ankles, don’t join the stubborn majority refusing treatment. Feel free to contact Pasquale Cancelliere, DPM from Candria Foot and Ankle Specialists. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is a Podiatrist?
Someone would seek the care of a podiatrist if they have suffered a foot injury or have common foot ailments such as heal spurs, bunions, arch problems, deformities, ingrown toenails, corns, foot and ankle problems, etc.
Podiatric Treatment
A podiatrist will treat the problematic areas of the feet, ankle or lower leg by prescribing the following:
- Physical therapy
- Drugs
- Orthotic inserts or soles
- Surgery on lower extremity fractures
A common podiatric procedure a podiatrist will use is a scanner or force plate which will allow the podiatrist to know the designs of orthotics. Patients are then told to follow a series of tasks to complete the treatment. The computer will scan the foot a see which areas show weight distribution and pressure points. The podiatrist will read the analysis and then determine which treatment plans are available.
If you have any questions please feel free to contact our offices located in Londonderry, NH and Salem, NH . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
What is a Podiatrist?
The branch of medicine that is focused on the treatment, diagnosis, and study of disorders of the lower leg, ankle and foot is referred to as podiatry. Because people often spend a great deal of their time on their feet, many problems in this area can occur. A person seeks help from the field of podiatry when they need treatment for heel spurs, bunions, arch problems, deformities, ingrown toenails, corns, foot and ankle problems, infections, and problems with the foot that are related to diabetes and additional diseases.
To treat problems of the foot, ankle or lower leg, a podiatrist may prescribe physical therapy, drugs, perform surgery, or set fractures. Individuals may also be recommended to wear corrective shoe inserts, custom-made shoes, plaster casts and strappings in order to correct deformities.
When trying to gather information on a patient problem, a scanner or force plate may be used in order to design orthotics. During this procedure, patients are told to walk across a plate that is connected to a computer; the computer then takes a scan of the foot and indicates weight distribution and pressure points. The computer readouts will give the podiatrist information to help them determine the correct treatment plans.
Diagnosis is also provided through laboratory tests and x-rays. Through the foot, the first signs of serious problems such as heart disease, diabetes and arthritis can show up. For example, individuals that have diabetes may frequently have problems such as infections and foot ulcers because they experience poor circulation in the foot area. A podiatrist can then have consultations with patients when symptoms arise. Referrals will then be made to specialists that handle the greater health problems.
Some podiatrists have their own independent, private practices or clinics where they have a small staff and administrative personnel. Many podiatrists work within group practices. They usually spend time performing surgery in ambulatory surgical centers or hospitals, or visit patients in nursing homes. Podiatrists typically spend between 30 to 60 hours of week working. Some podiatrists specialize in public health, orthopedics, surgery, or primary care. Other fields include specialties in geriatrics, dermatology, pediatrics, diabetic foot care and sports medicine.
Some podiatrist specialists complete extra training in the area of foot and ankle reconstruction that results from the effects of physical trauma or diabetes. There are also surgeons that perform surgery of a cosmetic nature to correct bunions and hammertoes.
Causes of Ankle Instability

Ankle instability can be a persistent and troublesome issue for many people, affecting their daily activities and overall quality of life. It often arises due to a variety of factors that compromise the stability of the ankle joint. One common cause of ankle instability is a history of ankle sprains. When an ankle is sprained, the ligaments that support it may stretch or tear, weakening its ability to hold the joint in place. Muscle weakness is another contributing factor, as insufficient strength in the muscles surrounding the ankle can increase the joint’s instability. Additionally, certain medical conditions, such as ligament laxity and joint hypermobility, can predispose individuals to ankle instability. Improper footwear choices, especially high heels or shoes lacking adequate support, can also strain the ankle joint over time. Finally, biomechanical issues like overpronation or supination can create an imbalance, which further increases the risk of ankle instability. If you're experiencing ankle instability, it is suggested that you make an appointment with a podiatrist for a personalized assessment and guidance on managing your condition.
Ankle pain can be caused by a number of problems and may be potentially serious. If you have ankle pain, consult with Pasquale Cancelliere, DPM from Candria Foot and Ankle Specialists. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
Ankle pain is any condition that causes pain in the ankle. Due to the fact that the ankle consists of tendons, muscles, bones, and ligaments, ankle pain can come from a number of different conditions.
Causes
The most common causes of ankle pain include:
- Types of arthritis (rheumatoid, osteoarthritis, and gout)
- Ankle sprains
- Broken ankles
- Achilles tendonitis
- Achilles tendon rupture
- Stress fractures
- Bursitis
- Tarsal tunnel syndrome
- Plantar fasciitis
Symptoms
Symptoms of ankle injury vary based upon the condition. Pain may include general pain and discomfort, swelling, aching, redness, bruising, burning or stabbing sensations, and/or loss of sensation.
Diagnosis
Due to the wide variety of potential causes of ankle pain, podiatrists will utilize a number of different methods to properly diagnose ankle pain. This can include asking for personal and family medical histories and of any recent injuries. Further diagnosis may include sensation tests, a physical examination, and potentially x-rays or other imaging tests.
Treatment
Just as the range of causes varies widely, so do treatments. Some more common treatments are rest, ice packs, keeping pressure off the foot, orthotics and braces, medication for inflammation and pain, and surgery.
If you have any questions, please feel free to contact our offices located in Londonderry, NH and Salem, NH . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Everything You Need to Know About Gout
Gout, typically found in diabetic patients, is an unusually painful form of arthritis caused by elevated levels of uric acid in the bloodstream. The condition typically strikes the big joint on the big toe. It has also been known to strike the knees, elbows, fingers, ankles and wrists—generally anywhere that has a functioning, moving joint.
The high level of uric acid in a person’s bloodstream creates the condition known as hyperuricema—the main cause of gout. Genetic predisposition occurs in nine out of ten sufferers. The children of parents who suffer gout will have a two in ten chance of developing the condition as well.
This form of arthritis, being particularly painful, is the leftover uric acid crystallizing in the blood stream. The crystallized uric acid then travels to the space between joints where they rub, causing friction when the patient moves. Symptoms include: pain, redness, swelling, and inflammation. Additional side effects may include fatigue and fever, although reports of these effects are very rare. Some patients have reported that pain may intensify when the temperature drops, such as when you sleep.
Most cases of gout are easily diagnosed by a podiatrist’s assessment of the various symptoms. Defined tests can also be performed. A blood test to detect elevated levels of uric acid is often used as well as an x-ray to diagnose visible and chronic gout.
Treatment for gout simply means eliminating symptoms. Non-steroid anti-inflammatory drugs or NSAIDs (Colchicine and other corticosteroid drugs, etc.) will quell the redness, the swelling, and the inflammation. However, managing your diet, lifestyle changes, and using preventative drugs are all helpful toward fully combating the most severe cases.
Those that lead an inactive lifestyle are at a higher risk for gout. Any amount of exercise decreases the probability of repeat encounters with the condition. Reducing your consumption of red meat, sea food, and fructose-sweetened drinks also reduces the likelihood of chronic gout as well.
Ingesting Vitamin C, coffee, and particular dairy products can help with maintaining a healthy lifestyle. There are new drugs out on the market that inhibit the body’s production of uric acid-producing enzymes. However, reducing or eliminating your overall levels of uric acid is the best remedy to ensuring you lead a gout-free life.
Symptoms and Treatment of Flat Feet

Flat feet, or pes planus, is a common condition where the arches of the feet collapse, causing the entire sole to touch the ground. This condition may be present from birth or develop over time. Genetics may play a significant role because the development of arches is determined by genetics. Insufficient development of foot muscles or weakening due to factors like aging or inactivity also can contribute to flat feet. Certain medical conditions like arthritis, diabetes, and obesity can increase the risk of developing flat feet. Some people experience no discomfort from flat feet, while others may suffer from pain in the arches or heels, swelling, or difficulty standing on tiptoes. Treatment options for flat feet depend on the severity and symptoms. Custom orthotic inserts can provide arch support and alleviate discomfort. Stretching exercises may help strengthen the foot muscles. In some cases, anti-inflammatory medication may be recommended. Early intervention can prevent further complications and improve your overall foot health. If you're experiencing flat feet-related issues, it's suggested that you consult a podiatrist for a thorough evaluation and a personalized treatment plan.
Flatfoot is a condition many people suffer from. If you have flat feet, contact Pasquale Cancelliere, DPM from Candria Foot and Ankle Specialists. Our doctor will treat your foot and ankle needs.
What Are Flat Feet?
Flatfoot is a condition in which the arch of the foot is depressed and the sole of the foot is almost completely in contact with the ground. About 20-30% of the population generally has flat feet because their arches never formed during growth.
Conditions & Problems:
Having flat feet makes it difficult to run or walk because of the stress placed on the ankles.
Alignment – The general alignment of your legs can be disrupted, because the ankles move inward which can cause major discomfort.
Knees – If you have complications with your knees, flat feet can be a contributor to arthritis in that area.
Symptoms
- Pain around the heel or arch area
- Trouble standing on the tip toe
- Swelling around the inside of the ankle
- Flat look to one or both feet
- Having your shoes feel uneven when worn
Treatment
If you are experiencing pain and stress on the foot you may weaken the posterior tibial tendon, which runs around the inside of the ankle.
If you have any questions please feel free to contact our offices located in Londonderry, NH and Salem, NH . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.