Dealing With Pressure Sores

Pressure sores on the feet develop when prolonged pressure restricts blood flow, causing tissue breakdown and open wounds. They are more likely in people with limited mobility, diabetes, or poor circulation, as the heel, ankle, and ball of the foot are frequent points of stress. Preventive measures focus on reducing pressure and friction on these areas. This includes using properly fitting shoes that provide adequate support, avoiding prolonged pressure from tight straps or flip-flops, and protecting bony prominences of the feet with cushioning materials. Podiatrists often recommend devices that redistribute weight across the sole, lowering the risk of ulcer formation. They also check for early warning signs such as redness, skin thinning, or changes in sensation, which signal developing sores. In advanced cases, untreated pressure sores can lead to infection, difficulty walking, or even limb loss if surgery becomes necessary. If you have developed pressure sores, it is suggested that you make an appointment with a podiatrist for an exam and treatment.
Wound care is an important part in dealing with diabetes. If you have diabetes and a foot wound or would like more information about wound care for diabetics, consult with Pasquale Cancelliere, DPM from Candria Foot and Ankle Specialists. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
What Is Wound Care?
Wound care is the practice of taking proper care of a wound. This can range from the smallest to the largest of wounds. While everyone can benefit from proper wound care, it is much more important for diabetics. Diabetics often suffer from poor blood circulation which causes wounds to heal much slower than they would in a non-diabetic.
What Is the Importance of Wound Care?
While it may not seem apparent with small ulcers on the foot, for diabetics, any size ulcer can become infected. Diabetics often also suffer from neuropathy, or nerve loss. This means they might not even feel when they have an ulcer on their foot. If the wound becomes severely infected, amputation may be necessary. Therefore, it is of the upmost importance to properly care for any and all foot wounds.
How to Care for Wounds
The best way to care for foot wounds is to prevent them. For diabetics, this means daily inspections of the feet for any signs of abnormalities or ulcers. It is also recommended to see a podiatrist several times a year for a foot inspection. If you do have an ulcer, run the wound under water to clear dirt from the wound; then apply antibiotic ointment to the wound and cover with a bandage. Bandages should be changed daily and keeping pressure off the wound is smart. It is advised to see a podiatrist, who can keep an eye on it.
If you have any questions please contact our offices located in Londonderry, NH and Salem, NH . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Wound Care
Diabetics must be wary of all wounds, regardless of depth or size. Diabetes, a chronic disease in which the body cannot properly use glucose the way it normally would, causes various complications that make wounds difficult to heal. Nerve damage or neuropathy will cause diabetics to have trouble feeling the pain of a blister or cut until the condition has significantly worsened or become infected. A diabetic’s weakened immune system can make even the most minor of wounds easily susceptible to infection. Diabetics are also more prone to developing narrow, clogged arteries, and are therefore more likely to develop wounds.
Wounds should be taken care of immediately after discovery, as even the smallest of wounds can become infected if enough bacteria build up within the wound. To remove dirt, wounds should be first rinsed under running water only. Soap, hydrogen peroxide, or iodine can irritate the injury and should be avoided. To prevent infection, apply antibiotic ointment to the wound and cover it with a bandage. The bandage should be changed daily. The skin around the wound may be cleaned with soap.
To prevent further exacerbation, see a doctor—especially if you have diabetes. Minor skin conditions can become larger problems if not properly inspected. As the wound heals, make sure to avoid applying pressure to the affected area.
Stages of Diabetic Foot Ulcers
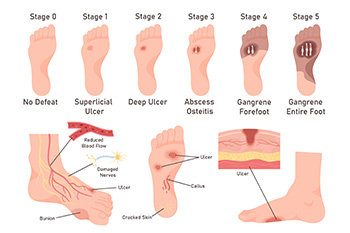
Diabetic foot ulcers often progress through stages that reflect increasing levels of tissue damage. In the earliest stage, the skin may appear intact, but deformities or poor circulation place the foot at risk for breakdown. A grade 1 ulcer is a shallow wound that affects only the skin’s outer layers. A grade 2 ulcer involves deeper tissues, such as tendons, ligaments, or joints. By grade 3, the ulcer may spread into the bone, creating a serious health concern. grade 4, involves dead tissue, or gangrene, at the front of the foot, and grade 5 occurs when gangrene extends throughout the entire foot, which can threaten limb preservation. A podiatrist can evaluate the severity of the diabetic foot ulcer, provide wound care, help improve circulation, and recommend surgery when necessary to reduce the risk of limb loss. If you have diabetes with developing foot ulcers, it is suggested that you schedule an appointment with a podiatrist for an exam and expert guidance in managing this serious condition.
Diabetic foot care is important in preventing foot ailments such as ulcers. If you are suffering from diabetes or have any other concerns about your feet, contact Pasquale Cancelliere, DPM from Candria Foot and Ankle Specialists. Our doctor can provide the care you need to keep you pain-free and on your feet.
Diabetic Foot Care
Diabetes affects millions of people every year. The condition can damage blood vessels in many parts of the body, especially the feet. Because of this, taking care of your feet is essential if you have diabetes, and having a podiatrist help monitor your foot health is highly recommended.
The Importance of Caring for Your Feet
- Routinely inspect your feet for bruises or sores.
- Wear socks that fit your feet comfortably.
- Wear comfortable shoes that provide adequate support.
Patients with diabetes should have their doctor monitor their blood levels, as blood sugar levels play such a huge role in diabetic care. Monitoring these levels on a regular basis is highly advised.
It is always best to inform your healthcare professional of any concerns you may have regarding your feet, especially for diabetic patients. Early treatment and routine foot examinations are keys to maintaining proper health, especially because severe complications can arise if proper treatment is not applied.
If you have any questions, please feel free to contact our offices located in Londonderry, NH and Salem, NH . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Diabetic Foot Care
Diabetes affects millions of people every year. Blood vessels located all over the body are damaged due to diabetes—even the blood vessels of the feet. Neuropathy, or nerve damage, can result from slower blood flow in the legs and feet. In diabetic patients, neuropathy is very important to monitor, as diabetics are at risk for developing ulcers.
Always washing and thoroughly drying the feet are pertinent parts of diabetic foot care. There should be a focus on cleaning between the toes. Even if no pain is felt, the entire foot should be examined for redness and sores. Neuropathy can often mask the pain of sores and ulcers and can cause these conditions to be overlooked. Use a mirror to examine the underside of your feet if needed. It is recommended that diabetics wear well-fitting socks.
Patients with diabetes should have their doctor monitor their blood levels because blood sugar levels play a huge role in diabetic care. Monitoring these levels on a regular basis is highly advised. It is very important to keep your blood sugar levels in the normal range, which can be determined by your physician. There are medications that may be prescribed to help with any neuropathy experienced by the diabetic patient. It is also advisable to visit a podiatrist if one is experiencing any conditions involving the feet, such as ingrown toenails, which in more severe cases can cause infection.
Diabetic feet must be inspected daily. Diabetic foot care at home is possible if a patient is provided with instructions from their podiatrist. Patients can relieve dry heels with creams or ointments. Suspected wounds should warrant an immediate call to the podiatrist. Gangrene is a serious problem for diabetics and can lead to sepsis and amputation in its worst cases. Early treatment and daily inspection of diabetic feet are keys to staying healthy.
Heel Lumps and What Causes Them

A lump on the heel is often linked to a condition known as Haglund’s deformity, where a bony prominence develops at the back of the heel bone. This extra bone growth can irritate the Achilles tendon and the bursa, a small fluid-filled sac that normally reduces friction. This can lead to swelling, redness, and localized pain. Contributing causes may include tight calf muscles that increase tension on the tendon, genetic factors like high arches that shift the heel bone backward, or footwear with a stiff backs like pumps, ice skates, or high heels that create repeated friction. A podiatrist can perform an exam to determine if the heel lump is related to bone spurs, bursitis, or tendon irritation. Treatment options include stretching exercises, changes in footwear, medication, and surgery, in persistent cases. If you notice the formation of a lump on the heel, it is suggested that you schedule an appointment with a podiatrist for appropriate treatment.
Many people suffer from bouts of heel pain. For more information, contact Pasquale Cancelliere, DPM of Candria Foot and Ankle Specialists. Our doctor can provide the care you need to keep you pain-free and on your feet.
Causes of Heel Pain
Heel pain is often associated with plantar fasciitis. The plantar fascia is a band of tissues that extends along the bottom of the foot. A rip or tear in this ligament can cause inflammation of the tissue.
Achilles tendonitis is another cause of heel pain. Inflammation of the Achilles tendon will cause pain from fractures and muscle tearing. Lack of flexibility is also another symptom.
Heel spurs are another cause of pain. When the tissues of the plantar fascia undergo a great deal of stress, it can lead to ligament separation from the heel bone, causing heel spurs.
Why Might Heel Pain Occur?
- Wearing ill-fitting shoes
- Wearing non-supportive shoes
- Weight change
- Excessive running
Treatments
Heel pain should be treated as soon as possible for immediate results. Keeping your feet in a stress-free environment will help. If you suffer from Achilles tendonitis or plantar fasciitis, applying ice will reduce the swelling. Stretching before an exercise like running will help the muscles. Using all these tips will help make heel pain a condition of the past.
If you have any questions, please feel free to contact our offices located in Londonderry, NH and Salem, NH . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Heel Pain
Heel pain can be difficult to deal with, especially if you do not know what the underlying cause is. If you ignore your heel pain, the pain can magnify and potentially develop into a chronic condition. Depending on the location of your heel pain, you have developed a specific condition.
One condition is plantar fasciitis. Plantar fasciitis is caused by the inflammation of the plantar fascia, or the band of tissue that connects the heel bone to the base of the toes. The pain from this condition is initially mild but can intensify as more steps are taken when you wake up in the morning. To treat this condition, medication will likely be necessary. Plantar fasciitis is often associated with heel spurs; both require rest and special stretching exercises.
There are various options your podiatrist may suggest for heel pain. Treatment options for heel pain typically include non-steroidal anti-inflammatory drugs (NSAIDS), which may reduce swelling and pain. Other options are physical therapy, athletic taping, and orthotics. In severe cases of heel pain, surgery may be required.
Preventing heel pain is possible. If you are looking to prevent heel pain from developing in the future, be sure to wear shoes that fit you properly and do not have worn down heels or soles. Be sure to warm up properly before participating in strenuous activities or sports that place a lot of a stress on the heels. If you are experiencing any form of heel pain, speak with your podiatrist to determine the underlying cause and receive the treatment you need.
Common Types of Athlete’s Foot

Athlete’s foot is a fungal infection that affects the skin on the feet, and usually occurs in three varieties called interdigital, moccasin, and vesicular. Interdigital athlete’s foot typically appears between the toes, causing itching, redness, peeling, and sometimes cracking or bleeding skin. Moccasin athlete’s foot affects the soles and sides of the feet, leading to dry, scaly, and thickened skin. Vesicular athlete’s foot is characterized by small, itchy blisters that may appear on the soles or insteps. Causes include walking barefoot in moist, communal areas, wearing damp socks, and poor foot hygiene. The infection can feel itchy, burning, or uncomfortable, and the affected skin may appear red, flaky, or cracked. A podiatrist can diagnose athlete’s foot through a physical examination and skin scrapings, if needed. Treatment may include antifungal creams, oral medications, and advice on prevention. To address symptoms effectively, it is suggested that you schedule an appointment with a podiatrist who can effectively treat athlete's foot.
Athlete’s Foot
Athlete’s foot is often an uncomfortable condition to experience. Thankfully, podiatrists specialize in treating athlete’s foot and offer the best treatment options. If you have any questions about athlete’s foot, consult with Pasquale Cancelliere, DPM from Candria Foot and Ankle Specialists. Our doctor will assess your condition and provide you with quality treatment.
What Is Athlete’s Foot?
Tinea pedis, more commonly known as athlete’s foot, is a non-serious and common fungal infection of the foot. Athlete’s foot is contagious and can be contracted by touching someone who has it or infected surfaces. The most common places contaminated by it are public showers, locker rooms, and swimming pools. Once contracted, it grows on feet that are left inside moist, dark, and warm shoes and socks.
Prevention
The most effective ways to prevent athlete’s foot include:
- Thoroughly washing and drying feet
- Avoid going barefoot in locker rooms and public showers
- Using shower shoes in public showers
- Wearing socks that allow the feet to breathe
- Changing socks and shoes frequently if you sweat a lot
Symptoms
Athlete’s foot initially occurs as a rash between the toes. However, if left undiagnosed, it can spread to the sides and bottom of the feet, toenails, and if touched by hand, the hands themselves. Symptoms include:
- Redness
- Burning
- Itching
- Scaly and peeling skin
Diagnosis and Treatment
Diagnosis is quick and easy. Skin samples will be taken and either viewed under a microscope or sent to a lab for testing. Sometimes, a podiatrist can diagnose it based on simply looking at it. Once confirmed, treatment options include oral and topical antifungal medications.
If you have any questions, please feel free to contact our offices located in Londonderry, NH and Salem, NH . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Athlete's Foot
Athlete’s foot is an extremely contagious infection caused by a fungus that results in itching, burning, dry, and flaking feet. The fungus that causes athlete’s foot is known as tinea pedis and thrives in moist, dark areas such as shower floors, gyms, socks and shoes, commons areas, public changing areas, bathrooms, dormitory style houses, locker rooms, and public swimming pools. Athlete’s foot is difficult to treat as well because of the highly contagious and recurrent nature of the fungus.
Tinea is the same fungus that causes ringworm, and is spread by direct contact with an infected body part, contaminated clothing, or by touching other objects and body parts that have been exposed to the fungus. Because the feet are an ideal place for tinea to grow and spread, this is the most commonly affected area. It is, however, known to grow in other places. The term athlete’s foot describes tinea that grows strictly on the feet.
The most commonly infected body parts are the hands, groin, and scalp, as well as the feet. Around 70% of the population suffer from tinea infections at some point in their lives, however not all of these cases are athlete’s foot. Just like any other ailment, some people are more likely to get it than others, such as people with a history of tinea infections or other skin infections, both recurring and non-recurring ones. The extent to which a person experiences regrowth and recurrent tinea infections varies from person to person.
Sometimes people will not even know that they are infected with tinea or that they have athlete’s foot because of a lack of symptoms. However, most experience mild to moderate flaking, itching, redness, and burning. However, some of the more severe symptoms include cracking and bleeding skin, intense itching and burning, pain while walking or standing, and even blistering.
Because of the recurring nature of the tinea fungus and the athlete’s foot it causes, the best way to treat this condition is with prevention. You can take some preventative measures such as wearing flip flops or sandals in locker rooms and public showers to reduce contact with the floor. It also helps to keep clean, dry feet while allowing them to breathe. Using powders to keep your feet dry is a good idea, as well as keeping your feet exposed to light and cool air, to prevent the growth of tinea. If you do happen to get athlete’s foot, opt for using topical medicated creams, ointments or sprays. These treatments help eliminate and prevent it from coming back.
Freiberg Infraction and Foot Pain

Freiberg infraction is a condition that affects the long bones in the front of the foot, most often the second metatarsal. It happens when the bone under the toe joint loses its normal blood supply, leading to tiny fractures and collapse of the bone surface. This can cause pain in the ball of the foot, swelling, and stiffness in the toe. Walking or wearing tight shoes may make the discomfort worse, and over time, the joint may become stiff or uneven. The condition is more common in teenagers and young adults, especially those who are active in sports, although adults can develop it, as well. Treatment may involve rest, wearing cushioned shoes, orthotics, or targeted exercises to relieve pressure and improve movement. Severe cases may require surgery. If you have persistent pain in the ball of your foot, it is suggested that you see a podiatrist for evaluation and appropriate treatment.
Some foot conditions may require additional professional care. If you have any concerns, contact Pasquale Cancelliere, DPM of Candria Foot and Ankle Specialists. Our doctor can provide the care you need to keep you pain-free and on your feet.
Rare Foot Conditions
The majority of foot conditions are common and can be treated by a podiatrist. Standard diagnostic procedures are generally used to identify specific conditions and treatment can be rendered. A podiatrist also treats rare foot conditions which can be difficult to diagnose and may need extra attention and care.
There are many rare foot conditions that can affect children. Some of these can include:
- Freiberg’s disease
- Kohler’s disease
- Maffucci syndrome
Freiberg’s disease - This can be seen as a deterioration and flattening of a metatarsal bone that exists in the ball of the foot. It typically affects pre-teen and teenage girls, but can affect anyone at any age. Symptoms that can accompany this can be swelling, stiffness, and the patient may limp.
Kohler’s disease - This often targets the bone in the arch of the foot and affects younger boys. It can lead to an interruption of the blood supply which ultimately can lead to bone deterioration. The patient may limp or experience tenderness, swelling, and redness.
Maffucci syndrome - This affects the long bones in a child’s foot leading to the development of abnormal bone lesions. They are benign growths and typically develop in early childhood and the bones may be susceptible to breaking.
A podiatrist can properly diagnose and treat all types of rare foot conditions. If your child is affected by any of these symptoms or conditions, please don’t hesitate to call our office so the correct treatment method can begin.
If you have any questions, please feel free to contact our offices located in Londonderry, NH and Salem, NH . We offer the newest diagnostic and treatment technologies for all your foot care needs.